LIMITED TIME OFFER SAVE UP TO 95% OFF ED MEDS & PAY $2 PER TABLET.
Talk to live agent (Mon – Fri: 9:30am – 6:30pm EST).
(866) 294-3772
More questions? Visit our FAQ page
Starting at $399 $199
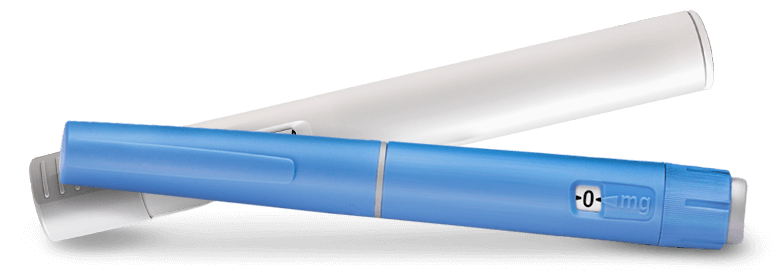
Same active ingredient in Wegovy®
& Ozempic® for a fraction of the price
Includes medication, healthcare
provider
& weight loss support
Semaglutide helps curb hunger,
keeping you feeling fuller
Weight loss medication Wegovy® is in low supply.
Get started with semaglutide, shipped overnight to your door. Now available through Rex MD®
Weight loss medication Wegovy® is in low supply.
Get started with semaglutide, shipped overnight to your door. Now available through Rex MD®

Verified Trustpilot
Rex MD Patient Rating
Patients Have Chosen
Rex MD for Telehealth
Online Completed
Rex MD Consultations

There’s no commitment to get started!
First, share your weight loss goals and health history with
your Rex MD affiliated provider through our confidential
online questionnaire.
Your Rex MD affiliated provider will review your results to
see if medication is right for you. The Rex MD Weight
Management Program includes access to
groundbreaking GLP-1 medications if appropriate,
and ongoing provider care to help you reach your
target weight.

Rex MD will send your prescription to the pharmacy and
have your GLP-1 medication shipped overnight, directly
to your door if approved by your dedicated Rex MD
affiliated provider.
Rex MD stands by your side every step of your journey,
starting from your initial dose to your first milestone
in reaching your weight loss goals.



There’s no commitment to get started!
To help cover medication cost, members receive
GLP-1 Medication Insurance Assistance

Everything you need for success
This program combines groundbreaking GLP-1 medications, lab testing (if needed), and the knowledge of leading clinicians to create a highly effective approach to weight loss. We'll take your unique metabolic profile and lifestyle habits into account to help ensure you lose that extra weight - one of the most important things you'll ever do for your health.
Yes! Everything, from your initial visit to support from clinicians and ongoing check-ins, can be done right from your computer or smartphone. Lab work may be required.
GLP-Is are groundbreaking medications that have shown remarkable results in clinical studies. GLP-1 medications help regulate and improve the body's weight loss factors - such as blood sugar response and insulin. By changing these factors, the gut will send signals to the brain to improve metabolic function and regulate digestion and appetite, helping patients feel fuller, longer. In studies, patients lost 15-20% of their body weight* with GLP-1 medication.
GLP-1’s typically come in either a prefilled injection pen that contains multiple doses, or a manual injection through vial and syringe. If it’s prescribed, you (or someone in your household) will select the prescribed dose, then administer the injection under the skin of your stomach, thigh, or arm once a week.
While a routine injection may sound intimidating, the pen uses a tiny needle designed to minimize discomfort. You’ll also receive clear instructions on using the injection pen, and your Rex MD affiliated provider can offer additional advice.
Licensed medical providers deliver comprehensive care, including your initial visit and ongoing medical check-ins from the comfort of your home. Lab work may be required.
Begin your journey to a healthier lifestyle with our exceptional offer: Our program is just $199 per month, with the flexibility to cancel anytime.
Helpful info to help you achieve your goal weight.
Helpful info to help you achieve your goal weight.
You’re now in control. Take the first step towards
more compliments, looking great in photos, baggy
clothes that no longer fit... and a healthier, happier,
more confident you!

TestoRx will be available in October 2024

Enter your info to be one of the first in line.
Thank you! We'll email you as soon as TestoRX is available to the general public.
In the meantime, check out all of the Men's Telehealth Treatments and Save 95% Off with generic Viagra & generic Cialis today.